Blood clots can lead to life-threatening heart attacks, strokes and pulmonary embolisms.
As if the respiratory complications with Covid-19 weren't worrying enough, doctors are also discovering the risk of blood clots from the coronavirus.
As the virus travels through the world and hits hard, word is starting to spread about patients who are full of clots in their brains, lungs, hearts and legs - and sometimes everywhere. To cite one example, in Los Angeles, a Broadway star's right leg was amputated due to severe clotting. As we can imagine, this is very scary and alarming, both for the patient and for the healthcare system.
While the healthcare community is still learning how COVID-19 attacks the body, it seems that a few factors are causing the increased risk of blood clots.
The mechanism of blood coagulation
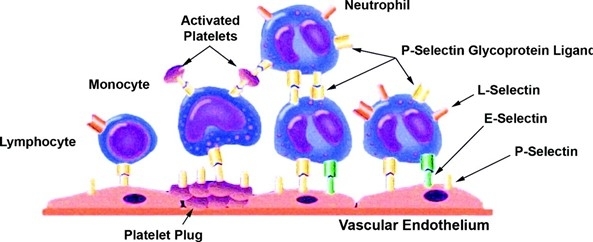
Immediately following endothelial cell injury (such as a small wound on your finger), endothelial cells and platelets are activated, promoting the expression of cell adhesion molecules (such as Catherins and Selectins). This vascular response promotes the rolling and tethering of leukocytes ( white blood cells) to the endothelium, which can trigger an inflammatory response, leading to thrombosis.
Factors that affect clotting
First, COVID-19 can cause severe inflammation, which can activate your clotting system. For example, if you fall and hurt your knee, your immune system is turned on and one of the ways your immune system responds to an injury is by making your clotting system more active. It makes sense that your body would say, "if I see an infection, I need to be ready to clot." But when the infection is as widespread and inflammatory as COVID-19, that tendency to clot can become dangerous for your body. And if you're sick with COVID-19 or following stay-at-home or quarantine rules, you're probably moving less. If you are immobile, you have an increased risk factor for forming blood clots.
Together, inflammation and immobility create a nearly perfect environment for blood clots in your legs and lungs. Patients with severe cases of COVID-19 seem particularly susceptible, as do those with other health risk factors such as cancer, obesity, and a history of blood clots.
Who is most at risk of blood clots and what can you watch out for?
Although those with severe cases of COVID-19 seem to suffer more from blood clots, those who do not need to go to the hospital may still be at risk. They, like everyone else, should watch for signs of blood clots and a possible stroke or heart attack such as:
- Hanging face
- Weakness of an arm or leg
- Difficulty speaking
- New swelling, tenderness, pain or discoloration in the arms or legs
- Sudden shortness of breath
- Chest pain or pain radiating to the arm, neck or jaw
Although some of the above symptoms occur unexpectedly , it is advisable to;
- Keep moving so the blood keeps flowing.
- Stay hydrated (drink a lot!).
- When you sit, try to keep your legs high.

Tests that have to do with blood clotting usually have to be taken directly at the lab and cannot be done at a decentralized blood collection point.
This concerns the tests such as d-dimer, INR, PT-INR, APPT
Blood tests that are related to blood coagulation and thrombosis and that can be administered decentrally are:
- With your iGene DNA test you can see if you have an increased risk of Thrombophilia (blood clotting)
- Cardiolipin: People with antibodies to cardiolipin have an increased risk of thrombosis
- A positive result for Lupus Anticoagulant: gives an increased risk of thrombosis
- The Factor V LEAD PCR test measures your genetic predisposition to thrombosis.
- Beta 2 Glycoprotein 1 antibodies occur in people with APS (increased risk of thrombosis and miscarriages)
- Always check your blood count too, this is part of most check-ups.
For the various corona tests see:



Tessa
Retrieved from Dec 15, 2021Julia
Retrieved from Dec 15, 2021