Are my thrombocytes elevated, is my hb too low, do I have too few platelets? All of these questions are answered by laboratory testing of the "blood count."
Many people think that a blood count gives a complete insight, but the blood count is just a small and inexpensive blood test.
There are hundreds of other parameters that can be determined, but the blood count already provides a lot of information. Want to know which ones? Then read on...
The blood test "complete blood count" is the most often performed of all possible tests, because it is a good starting point to find out what else is going on and to give direction to possible further research. The blood count is part of most check-ups.
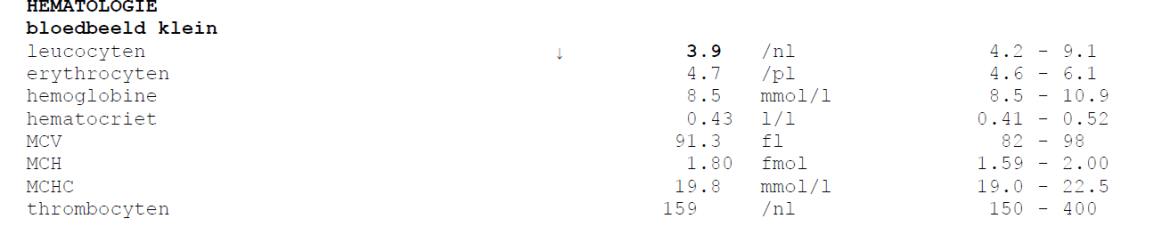
A blood count must be seen in context. If one of the components of the blood count deviates slightly, it does not necessarily mean anything. In case of an extremely low or high result requiring immediate medical intervention, you will always be called before receiving the result. Abnormal values are indicated by an up arrow ↑ for a high value and/or a down arrow ↓ for a low value.
A blood test remains a snapshot, sometimes it is wise to repeat the tests, which can be improved, after a month.
Blood value tests include a complete blood count and a large blood count. The large blood count also includes the leukocyte differentiation. Different labs use different names, such as complete blood count, blood smear, complete blood count (CBC), general blood count, extended blood count or complete blood count.
How is the blood obtained?
The blood is taken in the vessels, by a so-called venipuncture. Vacuum tubes with a precisely defined vacuum are used for this. This allows a certain volume of blood to be drawn off, so that the correct ratio between blood and anticoagulant can be achieved. It is customary to disinfect the puncture site, which is usually the crook of the elbow. A tourniquet is then placed around the upper arm, which causes the veins to swell visibly. Then the needle is inserted through the skin and the vessel wall, the tube is placed under the needle and the tourniquet is released. When the tube is full, a second tube can be filled. The tourniquet used for venipuncture is intended to make it easier to puncture a vessel. If the tourniquet is left in place during blood collection, while the pressure in the vessels is kept artificially high, undesirable changes occur in the composition of the blood to be analysed.
Blood collection methods.
Distinguish blood collection:
- Venous blood
- Capillary blood from the capillaries
It depends on the type of study how much and what type of blood needs to be drawn. Blood value test works with intravenous blood collection for blood count.
The living blood analysis is done with capillary blood (also called finger prick). This examination is scientifically controversial, also because it concerns the interpretation of a person who does the analysis by eye through a microscope. This is the reason why BloodValue Testing does not offer live blood analysis.
For venipuncture, we use vacuum tubes that have a precisely defined vacuum.
This allows a defined volume of blood to be drawn so that the correct ratio of blood to anticoagulant is achieved.
What could cause the results to be different?
- Prolonged search for veins.
- Push to fill the blood tube. Prolonged pushing increases concentration.
- Too rough a shake to mix the blood with the anticoagulant.
- Too long on the way to centrifugation, but transport has little or no effect on hemolysis.
- Reference values depend on age, gender and pregnancy.
- For the blood count it is not important whether you are sober or not, but for e.g. glucose it is.
- Medications may affect some rashes.
How does the research work?
The blood count is determined from an EDTA tube and is automatically analyzed on a machine in the lab.
This blood analysis takes place at the laboratory's haematology department.
A complete blood test involves measuring the average size, shape and number of red blood cells (erythrocytes) and white blood cells (leukocytes) in the blood sample and counting the number of platelets (thrombocytes). The measured values are compared to normal values. This blood test is done in an automated measuring system. If abnormalities are found, the blood will be further examined under the microscope.
In the past, blood was examined by smearing it on a slide and viewing this thin film of blood under the microscope. Because this method is rather labor intensive and involves variation in assessment, devices have been developed that can classify and count cells based on their size and structure.
The leukocyte differential, or " the diffje," is a simple blood test that provides information about which white blood cells are active. Together with the leukocyte count of the blood count, the test gives global information about whether and how long the patient has been ill and what kind of disease he might have. In Blood Value Testing, the small blood count + leukocyte count is called the large blood count.
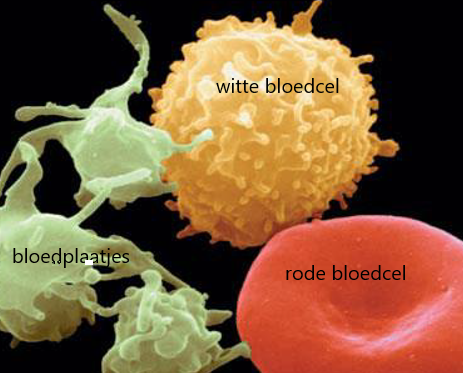
white blood cell = leucocyte
red blood cell = erythrocyte
platelets = thrombocyte
Leucocytes are the white blood cells
White blood cells (leukocytes) protect the body from infection. In the blood count test, the number and types of white blood cells are measured. There are five different types (neutrophils, lymphocytes, monocytes, eosinophils, and basophils), each with its own function. For example, an infection can increase the neutrophil count, an allergy can increase the eosinophil count, and a leukemia (blood cancer) can greatly increase the lymphocyte count.
Is it bad if your leucocytes are elevated? No, your leucocytes are the soldiers of your body and have to work when there is something to clear up, such as an infection. If you have an infection, you first see the number of white blood cells drop and then they are created for the attack and the number increases. We recognize dead white blood cells as pus. They died in the battle, but they saved your life.
Leukocytes (white blood cells).
- Colourless cells with a core
- Provide the immune defense and protect against pathogens such as viruses, bacteria and fungi, antibodies and clean up damaged own cells.
The Leukodiff provides information about the state of the body's immune system.
The white blood corpuscles exist for:
- 50-70% from Granulocytes (also known as neutrophils or neutrophilic granulocytes)
- 25-40% from Lymphocytes
- 1-5% from Eosinophilic granulocytes
- 0-3% from basophilic granulocytes
- 2-8% from Monocytes
Causes of elevated leukocytes are:
- Autoimmune diseases, e.g. allergies
- Bacterial or fungal infections
- Infarcts
- Leukaemia
- Metabolism disorders, (including thyroid diseases)
- Stress caused by inflammation
- Spleen removed
- Poisoning or too much toxicity
- Worm or parasite infections
Lymphocytosis is the name for greatly increased white blood cells, it occurs in: viral infections, toxoplasmosis, typhoid abdominalis, brucellosis, neoplastic diseases, acute or chronic lymphatic leukemia.
Causes of lowered leukocytes:
- Onset of viral, bacterial, yeast or parasite infection
- Spleen actively strengthened
- Irradiation of tumours (must not fall below 3.0 per nanoliter)
- Medication use
- Disturbed intestinal flora
- B12 deficiency
Lymphocytopenia is the name for the shortage of white blood cells, this occurs with a weakened immune system, HIV infection, chemotherapy, radiation, Lupes (SLE) erythematosus, tuberculosis, uremia (kidney failure), Cushing's disease, treatment with steroids, intestinal inflammatory diseases.
Please note, do not compare apples to oranges! Each test is reported in a certain unit. You can only compare your result to the reference values mentioned on your lab report. One lab reports in percent, the other in mmol/l meaning millimoles per liter, or the number measured per nanoliter or per picoliter.
Leucocytes- non scientific interpretation:
Increased leukocytes
Strengthened resistance
Communicatively problematic
Aggression and anger
Bile dysfunction, digestive problems from the small intestine
Autoimmune diseases, e.g. Hashimoto
Iron-copper ratio out of balance
Decreased leukocytes
Is open to external influences
Unable to set boundaries
Not steadfast and little perseverance
Erythrocytes are the red blood cells
Red blood cells (erythrocytes) contain the oxygen-transporting protein hemoglobin. If insufficient red blood cells are present, it may indicate anemia. If there are too many, polycytemia is present. However, this is rare. An abnormal increase in the number of red blood cells is also seen in heavy smokers, because chronic carbon monoxide poisoning makes the body think it is not getting enough oxygen and therefore makes extra red blood cells.
Normally red blood cells have almost the same size and shape, deviations can be caused by for example a lack of vitamin B12, folic acid or iron. The amount of hemoglobin is also determined, which can be used to assess whether enough oxygen is distributed throughout the body. The hematocrit measurement gives information about the volume that red blood cells occupy in the blood.
Red blood cells make up the largest proportion of blood cells. They are produced in the bone marrow. The kidneys are needed to produce red blood cells.
Because the kidneys produce the hormone EPO (erythropoietin), the bone marrow produces new red blood cells, which keeps blood levels up.
Kidneys may therefore interfere with Epo production.
The production of red blood cells requires iron, vitamin B12 and folic acid. After about 120 days the red blood cells are broken down by the spleen. Red blood cells consist of about 1/3 of the red pigment hemoglobin. They transport the oxygen from your lungs to the tissues. This blood value is also used to diagnose anaemia.
Increased red blood cell count
Symptoms:
- You don't notice much if the red blood cells are too high.
- It is a reaction of the body to compensate for a lack of oxygen.
Causes:
- Abnormal production of blood corpuscles.
- Oxygen deprivation due to stay in high mountains.
- Smoking (hemoglobin is occupied by the CO2 present in tobacco smoke).
- Severe heart problems (chronic lack of oxygen with a compensating effect on the production of erythrocytes).
- Tumours (often in kidney and liver carcinomas).
- Kidney diseases.
- Metabolic diseases; e.g., Cushing's syndrome (chronically elevated cortisol).
- Hormone therapies or administration of performance-enhancing drugs ( Testosterone, EPO, Cortisol).
Red cells - non scientific information
Decreased red blood cells:
Low energy (anergic), loss of chi
Mental/cognitive limitations
Limited perseverance
unhappy
MCV says something about the size of the red blood cells
MCV (Mean Corpuscular Volume) is the English term for the average size of red blood cells. An MCV that is too high is associated with anemia caused by vitamin B12 deficiency. An MCV that is too low is associated with iron deficiency anemia.
It is calculated by dividing all blood cells by the number of red blood cells.
High MCV occurs in:
- Vitamin B12 and folic acid deficiency
- Slow thyroid
- Liver Diseases
- Limited cell division and renewal
Low MCV occurs in:
- Iron and/or copper deficiency
- Vitamin B6 deficiency
MCV -non-scientific meaning
Lowered MCV
Not living from your authentic self
you make yourself "small"
You're not using your full potential
you're addiction- and depression-prone
Low energy (B6 and copper deficiency)
The MCV is also too low in patients with thalassemia (hereditary defect of the hemoglobin protein in the red blood cells).
MCH says how much oxygen the red blood cells can carry
MCH (Mean Corpuscular Hemoglobin) is the English term for calculating the amount of oxygen-carrying hemoglobin in red blood cells.
MCH is the mean cellular hemoglobin level.
A High MCH value occurs in:
- Vitamin B12 and folic acid deficiency
- A high MCH value is always the result of a lack of something.
Low MCH value occurs in:
- Iron and/or copper deficiency
- Vitamin B6 deficiency
- a lack of anything
MCH -Non-Scientific
Reduced and increased MCH
Lack of enjoyment of life
Unable or unwilling to enjoy
Does not live from his harmonious center
MCHC: how much Hb is in your red blood cells?
Mean Corpuscular Hemoglobin Concentration is the English term for calculating the hemoglobin concentration in red blood cells.
- MCHC mean cellular hemoglobin concentration
- Differential diagnosis of interest in severe anaemia
Such a calculation should never be interpreted in isolation, it should always be seen as part of the overall blood picture.
The result is optimal when the EDTA blood has reached the lab within 24 hours at room temperature. Small deviations can always occur without significance.
MCHC normal: in many forms of anemia, the MCHC is still normal.
MCHC reduced: possibly anaemia due to lack of iron or b12.
MCHC elevated: cold agglutinins: a form of hemolytic anemia caused by autoantibodies or spherocytosis:
Congenital spherocytosis is an inherited form of anemia. The cause is a change in the DNA, our genetic material. This causes the shape of red blood cells to be different.
Red blood cells carry oxygen through the body. Because of the different form, the body in someone with congenital spherocystosis breaks down red blood cells too quickly. This is done by the spleen. The spleen is an organ that determines which red blood cells still work properly and which do not. The spleen lies behind the stomach.
The characteristics of congenital spherocytosis vary from person to person. Some people are completely unaffected. Because the body breaks down too many red blood cells in congenital spherocytosis, anaemia can occur. This can cause, among other things, a person to look pale or feel awake or tired. Jaundice is also common, especially shortly after birth. This is when the eyes and skin turn a yellow colour. People with congenital spherocytosis also often have an enlarged spleen. Gallstones, short stature, and skeletal abnormalities are also common.
RDW(Relative Distribution Width) is the English term for calculating the variation in the size of red blood cells. In some types of anemia, there is a large variation in the size of red blood cells. Then the RDW is increased.
Hemoglobin transports the oxygen through your body
- Serves as a transport of oxygen and carbon dioxide
- After use by erythrocytes, hemoglobin is broken down into bile dye, iron and globin
Lime dye gives stool its typical color
Causes of elevated or reduced haemoglobin
Increased haemoglobin
- See "elevated erythrocyte value
Lowered hemoglobin
- See "lowered erythrocyte value.
- Iron deficiency
When increasing or decreasing, always consider:
- Smoking
- Excessive physical exertion
- Intensive sunbathing
- Medication
- Toxin load, e.g. PCB
- Testosterone substitution

Haemoglobin -non-scientific meaning
Lowered hemoglobin
Loss of inner stability
Basic dissatisfaction
Seeks reward through addictive behaviors, e.g., "I'm not a good person.
Food, alcohol, drugs, shopping sprees...
The normal values (reference values) of haemoglobin depend among other things on age and sex.
Elevated hemoglobin can result from:
- dehydration
- increased production of red blood cells in the bone marrow
- serious lung diseases
- Prolonged stay at high altitude (>2000 metres)
A lowered hemoglobin can be the result of:
- iron deficiency or lack of vitamins folic acid and B12
- hereditary haemoglobin disorders such as sickle cell anaemia or thallassemia
- genetic disorders of red blood cells
- liver decomposition (liver cirrhosis)
- excessive bleeding
- increased breakdown of red blood cells
- kidney diseases
- chronic inflammatory diseases
- malfunctioning bone marrow (aplastic anemia)
Hematocrit says something about the space your red blood cells take up in your blood.
The hematocrit measurement gives information about the volume of blood cells in the blood.
A lowered hematocrit indicates anemia, for instance caused by iron deficiency. Other causes of a low hematocrit can be vitamin deficiency, bleeding, liver disease or cancer. Further examination is necessary to find the cause of the anemia.
- an absolute or relative reduction in the erythrocyte count (all forms of anaemia)
- too much water in the body (dilution)
- pregnancy
Elevated hematocrit is usually caused by dehydration. Intake of sufficient fluids usually solves this problem. Another cause of a high hematocrit can be the disease polycytemia vera. In this disease too many red blood cells are produced in the bone marrow. High haematocrit can also occur when the lungs don't function properly, causing the body to lack oxygen. To compensate for this lack of oxygen, the bone marrow produces more red blood cells, which leads to an increased haematocrit.
- increase in the number of blood cells (polyglobulia)
- dehydration
- splenomegaly (enlarged spleen)
- tumors
- chronic infections
- higher cardiac load and circulatory disturbance in the tissue
Hematocrit non-scientific interpretation
Increased haematocrit
Slow thinking
Slow metabolism
Decreased haematocrit
Quick thinking and inability to hold thoughts
Fast metabolism
Platelets (thrombocytes)
Platelets play an important role in blood clotting. In the examination, the exact number of platelets is measured. If the number of platelets is too high, the risk of blood clots increases and if the number is too low, bleeding can easily occur (bruising). Infections and inflammations, iron deficiency and spleen removal can temporarily increase the number of thrombocytes. Sometimes a high thrombocyte count occurs for no apparent reason and without consequences. Thrombocyte counts can also be elevated in certain bone marrow diseases. In these bone marrow diseases, excessive bleeding as well as the easy formation of a clot (thrombosis) can occur. A low thrombocyte count can be caused by reduced production of thrombocytes in the bone marrow or by accelerated breakdown in the blood. In both cases, the thrombocyte count can become so low that bleeding occurs spontaneously.
Platelets are formed in the bone marrow and broken down again in the spleen after about 10 days. They do not possess a cell nucleus, they play a key role in blood coagulation.
When there is bleeding, the platelets release serotonin to support the contraction of the blood vessels. Thus, blood loss is minimized.
- Average platelet count is expressed as MPV value
Important to diagnose or control blood coagulation tendency
Elevated thrombocytes:
- Spleen removal (Splenectomy)
- Greater injuries
- After birth
- Infectious diseases
- severe iron deficiency
- After strenuous sporting activity / heavy physical exertion
- Very high thrombocytes can indicate leukaemia
- If the result is very high, there is an increased risk of vascular occlusion or thrombosis.
Decreased thrombocytes
- Virus infections
- Reduced blood formation (Erythrocytes and leukocytes are simultaneously reduced)
- Vitamin B12 deficiency
- Damage to the bone marrow
- Chemotherapy, radiation
- Heavy metals, in particular lead
- GSM radiation
- Medication; rheumatism and hormone preparations, diuretics
- Very low thrombocytes, there is an increased risk of bleeding. You can recognize bleeding in the skin (pinpoint bleeding) as small dots in the skin. These are small haemorrhages in the skin of the arms, legs, abdomen or buttocks. However, they can also occur in organs.
Platelets - non scientific interpretation
Increased platelets
Unresolved trauma
Emotional blockages
Shutting up for love
Always biased, overly critical, can't accept something
Guilt
Decreased thrombocytes
Is open to external influences
Unable to set boundaries
Very open-minded
Download an example result here
RDW-CV
RDW-CV stands for Red Cell Disbtribution Width - Coefficient of Variation. It is a laboratory test used to provide information on the variability and size of red blood cells in the blood.
A normal RDW-CV value reflects that the red blood cells are relatively uniform in size. However, if the RDW-CV value is too high, it may indicate a wider range of different size red blood cells, which may indicate certain medical conditions. Examples may include anemia, vitamin deficiency, bone marrow problems, inflammation, etc.
It is important to note that RDW-CV by itself is not diagnostic, but rather is a complementary test used in conjunction with other blood tests to get a more complete picture of a person's health status. If you have concerns about your RDW-CV value or other blood values, it is advisable to discuss it with a medical professional.
Differentiation of anemia forms from MCV and EBV (RDW)
MCV | RDW | Anemia Form | Possible cause |
Increased | Increased | Macrocytic anemia with anisocytosis | Vitamin B12 deficiency and/or folic acid deficiency |
Increased | Normal | Macrocytic anemia without anisocytosis | Panmyelopathy, displacement of erythropoiesis in the bone marrow-medication, bone marrow damage from ionizing radiation |
Normal | Increased | Normocytic anemia with anisocytosis | Incipient iron deficiency hemolytic anemia |
Normal | Normal | Normozytäre Anamia without anisocytosis | Chronic diseases renal failure, inflammation, maldigestion blood loss |
Lowered | Increased | Microcytic anemia with anisocytosis | Iron, copper and vitamin B6 deficiency Hemoglobinopathy |
Lowered | Normal | Microcytic anemia | Thalassaemia syndrome |
Anemia
Anemia can also be the result of, for example:
- Acute blood loss due to an accident, surgery, childbirth or chronic blood loss due to heavy menstruation or an inflammation or tumor in the gastrointestinal tract and urinary tract.
- Besides an increased loss of red blood cells, it can also be that insufficient blood cells are produced. This is usually caused by a shortage of iron, but a shortage of vitamin B12 or folic acid can also be the culprit. Poor diet is rarely the cause of anemia in the Netherlands. When you eat a healthy and varied diet, you get enough building blocks to make red blood cells. Pregnant women and growing children may have an increased need. There are also conditions that prevent the production of red blood cells. For example, there are disorders that suppress healthy bone marrow, thus compromising the production of blood cells (leukaemia) and sometimes not enough red blood cells are formed in the bone marrow (aplastic anaemia).
- A third cause of anemia is an increased breakdown of red blood cells. This is also called hemolytic anemia. In this case the blood cells are destroyed before their normal life span (120 days) has expired. This breakdown occurs faster than the bone marrow can replace the red blood cells. There are hereditary and non-hereditary forms of hemolytic anemia. Examples of hereditary forms are sickle cell disease and thalassemia. The non-hereditary form is caused by a lack of certain proteins or by a reaction of the immune system. Malaria, ticks or snake poison can also cause this form of anemia.
A Look into Your Resistance with the NLR Value
In addition to the usual markers in your blood count, there is another interesting measure that is often overlooked: the NLR value, or the neutrophil-to-lymphocyte ratio. This value offers insight into the balance between two key players in your immune system - neutrophils, which are the front line against infections, and lymphocytes, which are part of your adaptive immune system.
How Do You Calculate NLR?
It's surprisingly simple. You divide the number of neutrophils by the number of lymphocytes, both obtained from a standard complete blood count.
Why is NLR Important for Your Resistance?
The NLR reading is like a window on your immune system. A higher reading can be a sign of inflammation or stress in the body. It is a useful clue for doctors to dig deeper, especially if you are fighting an infection or wondering how strong your immune system is.
What Does an Abnormal NLR Mean?
An NLR that falls outside the norm is not cause for concern on its own. It is a signal that more may be going on, and it can help your doctor decide on possible next steps, such as additional testing or lifestyle changes.
Keeping an eye on the NLR level, along with the other components of your blood count, gives you a more complete picture of your overall health and resistance. It is a simple, yet powerful way to gain insight into how your body is functioning and responding to outside challenges.
Needless to worry?
So it is always important to consider carefully whether you want to have a check-up, because even such a small and standard blood test as the blood count can provide information that you might not want.
Read the information brochure from the GP Society here.
The individual values of the blood count should always be seen in combination and interpreted by a physician.
For example, blood cancer. This type of cancer originates in the lymph nodes. Another word for blood cancer is leukemia. Chronic lymphatic leukemia is also abbreviated to CLL. This type usually shows that the white blood cells increase over time. So if you look every 6 months you will see the white blood cells slowly increase, unlike with acute inflammation, where the white blood cells are elevated once.
CLL is the most common form of leukaemia in the Netherlands. About 600 people contract CLL each year. The disease is most common in people over the age of 60. But younger people can also get the disease. In men it occurs twice as often as in women.
CLL does not develop in the same way in every patient. About half of all patients have no symptoms. In these people, the disease is discovered by chance, for example during a routine examination, check-up or preventive medical examination. The disease progresses slowly in them. They do not need to be treated for the first 10-15 years. Of course, they do need periodic check-ups. Usually these people eventually die of causes other than CLL in old age. The other half of patients have mild symptoms. These increase over the years due to swelling of the lymph nodes, enlargement of the spleen, and decrease in blood cells. These patients are eventually treated to reduce the symptoms.
Do not draw any conclusions yourself from the blood picture. If something serious is going on, a manual examination under the microscope and an interpretation by the lab will follow. If something serious is going on, we will always call you first. So always give us your 06 number when you order, it will only be used for this!
Want to know how your blood count is?
In the medical check-up, other crucial blood values are measured in addition to the blood count: